What Is A Soap Note In Medical Terms . the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. documenting a patient assessment in the notes is something all medical students need to. soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient.
from positivepsychology.com
the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a standardized method for documenting patient information in healthcare. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. documenting a patient assessment in the notes is something all medical students need to. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient.
What are SOAP Notes in Counseling? (+ Examples)
What Is A Soap Note In Medical Terms soap notes are a standardized method for documenting patient information in healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a standardized method for documenting patient information in healthcare. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. documenting a patient assessment in the notes is something all medical students need to. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient.
From studylib.net
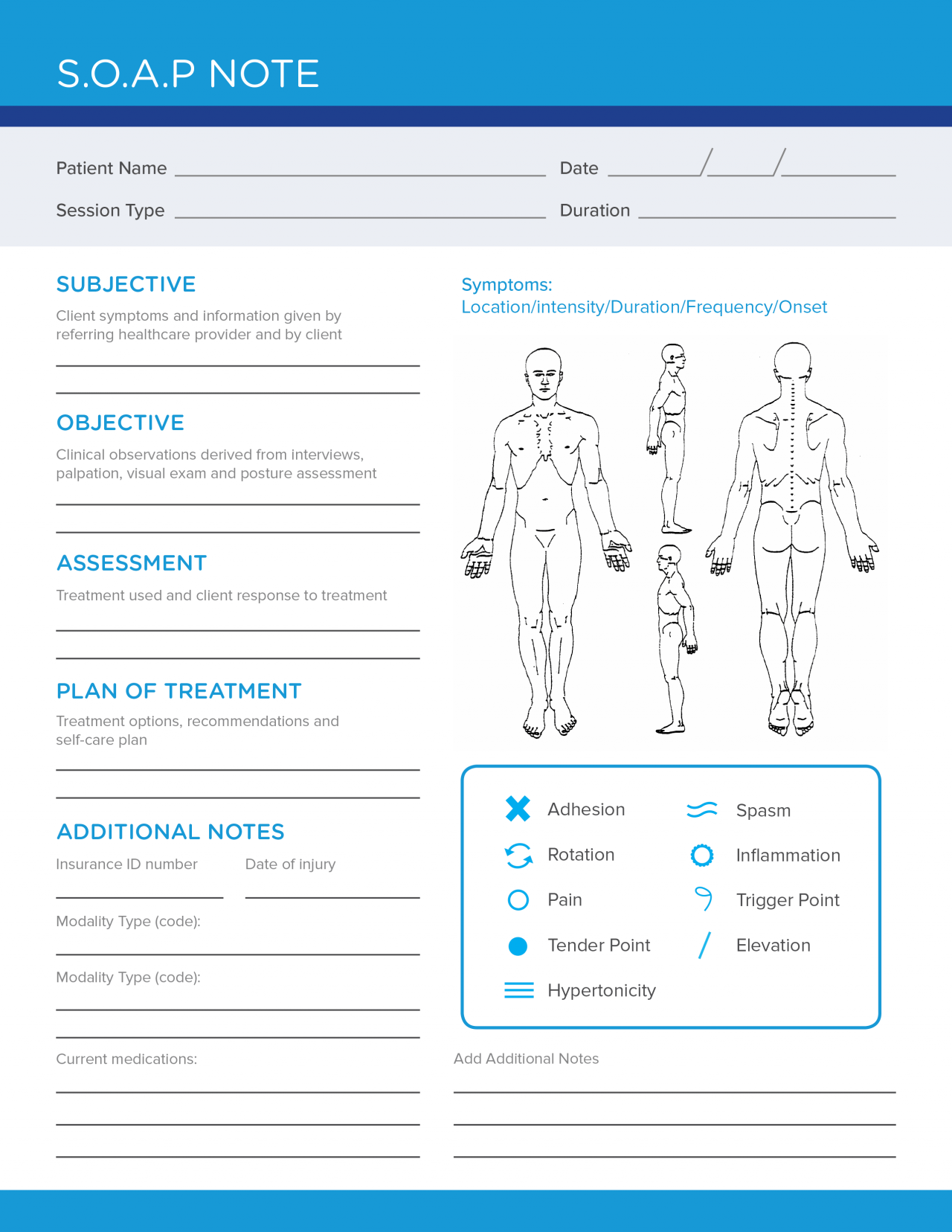
Patient SOAP Note Charting Procedures What Is A Soap Note In Medical Terms soap notes are a way for healthcare providers to document patient data more efficiently and consistently. documenting a patient assessment in the notes is something all medical students need to. soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap. What Is A Soap Note In Medical Terms.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab What Is A Soap Note In Medical Terms soap notes are a way for healthcare providers to document patient data more efficiently and consistently. documenting a patient assessment in the notes is something all medical students need to. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a standardized method for documenting patient information in. What Is A Soap Note In Medical Terms.
From canadianpa.ca
How to write a SOAP note — CANADIAN PA What Is A Soap Note In Medical Terms soap notes are a way for healthcare providers to document patient data more efficiently and consistently. documenting a patient assessment in the notes is something all medical students need to. soap notes are a standardized method for documenting patient information in healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. What Is A Soap Note In Medical Terms.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is A Soap Note In Medical Terms documenting a patient assessment in the notes is something all medical students need to. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a way for healthcare providers to document patient data. What Is A Soap Note In Medical Terms.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Is A Soap Note In Medical Terms soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method for documenting patient information in healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a. What Is A Soap Note In Medical Terms.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is A Soap Note In Medical Terms soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method for documenting patient information in healthcare. . What Is A Soap Note In Medical Terms.
From www.pinterest.com
Soap Note Example Nurse Practitioner All You Need To Know Soap note, Nursing notes examples What Is A Soap Note In Medical Terms the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. documenting a patient assessment in the notes is something all medical students need to. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method for documenting patient information in. What Is A Soap Note In Medical Terms.
From www.examples.com
Medical SOAP Note 10+ Examples, Format, How to write, Pdf What Is A Soap Note In Medical Terms the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap. What Is A Soap Note In Medical Terms.
From dxojjfbhy.blob.core.windows.net
Soap Note Example Medical at Mary Allen blog What Is A Soap Note In Medical Terms soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method for documenting patient information. What Is A Soap Note In Medical Terms.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is A Soap Note In Medical Terms soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. the subjective, objective, assessment and plan (soap) note is an acronym representing a. What Is A Soap Note In Medical Terms.
From positivepsychology.com
What are SOAP Notes in Counseling? (+ Examples) What Is A Soap Note In Medical Terms soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. . What Is A Soap Note In Medical Terms.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide What Is A Soap Note In Medical Terms soap notes are a standardized method for documenting patient information in healthcare. documenting a patient assessment in the notes is something all medical students need to. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes. What Is A Soap Note In Medical Terms.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is A Soap Note In Medical Terms soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. documenting a patient assessment in the notes is something all medical students need to. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap. What Is A Soap Note In Medical Terms.
From dev.ems-ce.com
Occupational Therapy Soap Note Template What Is A Soap Note In Medical Terms documenting a patient assessment in the notes is something all medical students need to. soap notes are a standardized method for documenting patient information in healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes. What Is A Soap Note In Medical Terms.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab What Is A Soap Note In Medical Terms documenting a patient assessment in the notes is something all medical students need to. soap notes are a standardized method for documenting patient information in healthcare. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. the. What Is A Soap Note In Medical Terms.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Note In Medical Terms soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes are a standardized method for documenting patient information in healthcare. soap notes are a way for healthcare providers to document patient data more efficiently and consistently. . What Is A Soap Note In Medical Terms.
From swimmingfreestyle.net
30 Medical soap Note Template Example Document Template What Is A Soap Note In Medical Terms soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method for documenting patient information in healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. documenting a patient assessment in the notes is something all medical students need. What Is A Soap Note In Medical Terms.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Note In Medical Terms soap notes are a way for healthcare providers to document patient data more efficiently and consistently. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes are a standardized method for documenting patient information in healthcare. . What Is A Soap Note In Medical Terms.